When to Provide Pastoral Support, When to Refer to a Licensed Counselor, and How to Do It Well
Ministry leaders are often the first place someone turns when life falls apart. That’s a sacred trust—and it’s also why clarity about scope matters.
This guide is designed to help pastors and ministry teams:
- know what’s within pastoral care / discipleship scope
- recognize red flags that require clinical care
- create a simple referral pathway that protects people
- strengthen collaboration between church and clinicians
This is not a “church vs. therapy” post. (We are so done with that narrative.) It’s a both/and approach: the healthiest path forward is clarity + collaboration + humility about scope.
Why this matters: words shape expectations
Many churches use the word counseling to describe discipleship or pastoral care. But in the public mind, “counseling” often implies licensed clinical mental health care—assessment, treatment planning, evidence-based interventions, ethical/legal standards, and professional accountability.
When those lanes blur, well-intended help can become confusing—or, in certain situations, unsafe.
Faith leaders are frequently a first point of contact in times of crisis, which makes having a clear plan even more important.
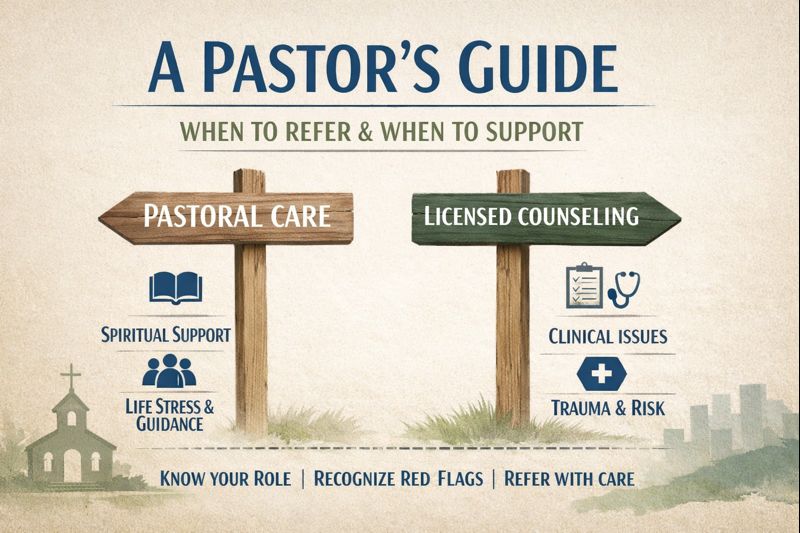
The Big Picture: Two Lanes, One Goal
Lane 1: Pastoral care / discipleship
Pastoral care is spiritually focused support, such as:
- prayer, Scripture, worship, community care
- encouragement, meaning-making, hope
- guidance for spiritual practices and relationships
- short-term support during life stressors (grief, conflict, transitions)
Lane 2: Clinical counseling (therapy)
Clinical care is healthcare. Licensed clinicians provide:
- assessment and treatment planning
- evidence-based interventions
- evaluation of risk (self-harm/suicide, abuse, crisis)
- documentation, confidentiality standards, informed consent
- ethical oversight and accountability through boards and licensure
The Pastor’s Scope of Practice: What’s In-Bounds vs. Out-of-Scope
In-bounds for most ministry leaders
Pastoral care can be a great first step when:
- the person is safe (no imminent risk)
- the concern is primarily spiritual formation
- symptoms are mild/moderate and daily functioning is normal
- you are offering short-term care (not ongoing appointments for months)
- you have clear boundaries and a referral plan if symptoms intensify
Examples:
- grief support and prayer
- marriage encouragement (not high-conflict, ongoing dynamics)
- spiritual doubt / deconstruction support
- loneliness, burnout, identity questions
- normal stress/anxiety around major transitions
Out-of-scope (refer to licensed clinical care)
A faith leader should promptly refer when there is a safety risk, severe symptoms, or complex clinical issues that require assessment and treatment planning. The APA Foundation’s faith leader guide includes clear “when to refer” guidance—especially when there is danger to self/others or serious behavioral/emotional impairment.
Referral Triage System (Simple + Usable)
Level 1: Emergency referral (right now)
If any of these are present:
- active suicidal intent, plan, or immediate danger
- threats of violence toward others
- psychosis, severe intoxication, or inability to care for self
- imminent domestic violence danger
What to do:
- Call emergency services (911)
- Do not leave the person alone if they are in imminent danger (follow your church’s safety policy)
Level 2: Referral to Licensed Counselor
Refer if:
- escalating panic attacks, inability to work/parent/function
- severe depression, hopelessness, major sleep disruption
- trauma symptoms after a recent event
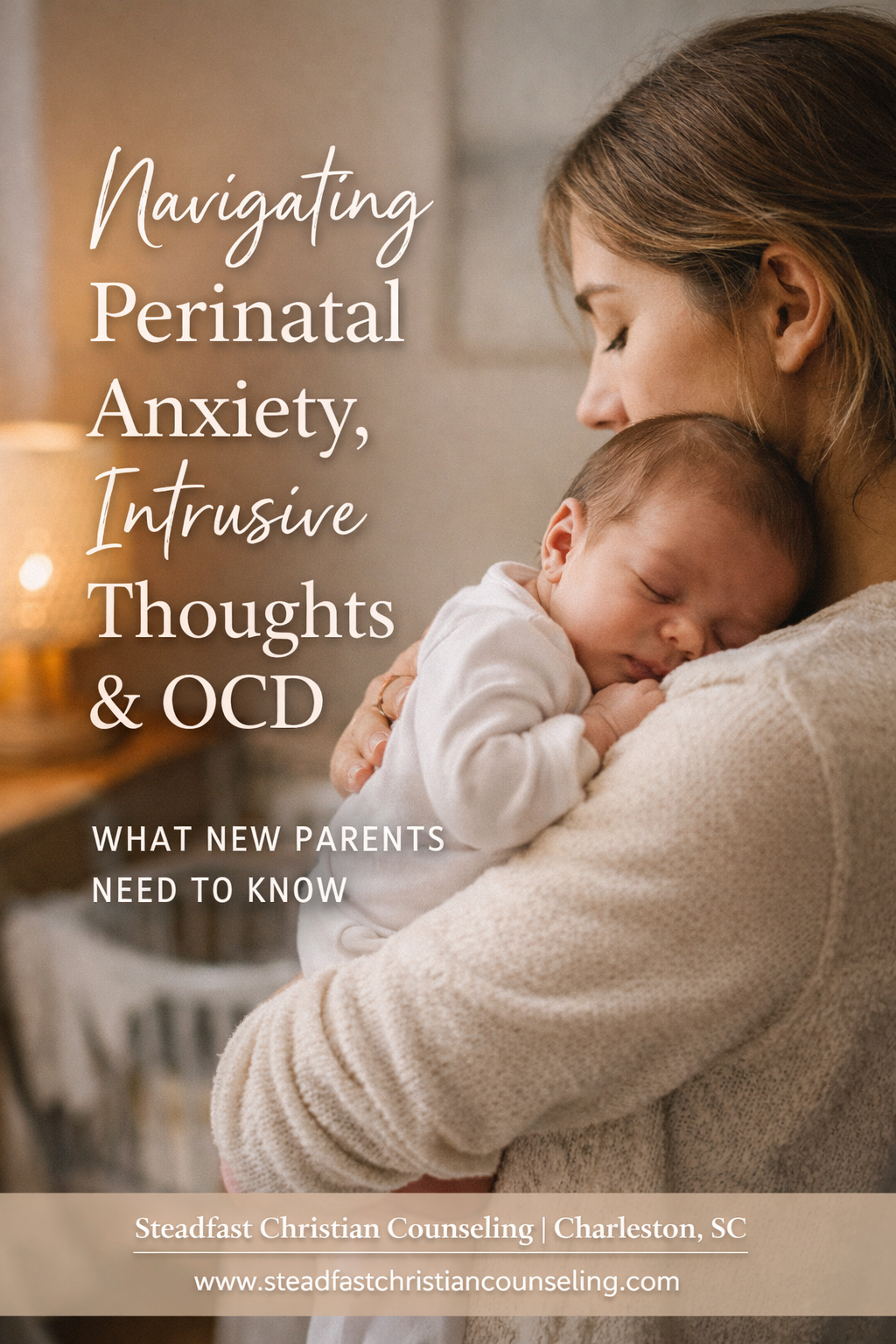
- postpartum anxiety/depression/intrusive thoughts that are distressing
- strong suspicion of OCD (example that may show up in your office: religious fears that you can’t help with rationally + compulsive behaviors – constantly needing the reassurance of prayer with you or at prayer-time after service)
- you suspect that counseling would be beneficial, but there’s no immediate risk
- patterns are entrenched (years of relational conflict, chronic anxiety, long-term trauma)
- pastoral care has been offered but symptoms persist
- addiction, eating disorders, severe self-neglect
- domestic abuse / coercive control indicators
- you’ve met multiple times and it’s becoming weekly long-term “therapy”
- you feel responsible for their stability
- they are dependent on you and avoiding professional help
- you’re outside your training (trauma, abuse, suicidality, OCD, addiction)
Language to Use When Referring
A referral script pastors can use (warm + clear)
“I’m really glad you told me. I want to support you spiritually—and I also want you to have the kind of care that matches what you’re carrying. Part of my responsibility as your pastor is to guide you to resources that I believe would help, and I have a list of a few licensed counselors in the city that I know that have the tools to give you some relief in these areas. I want you to know you are not broken, and God has given us so many tools that we can use to move through healing. What you are carrying is uncomfortable, but common, and there are tools that can help you. I’d love to stay in your corner spiritually while we get you connected to a counselor, as well.”
A Simple Referral Pathway Every Church Can Implement
Step 1: Build a vetted referral list and train teams well
Include:
- 2–3 trusted counseling practices (never just refer to one place – not ethical) (find practices that are trauma-informed, clinically serious, and ethically practicing within scope)
- crisis resources ( mobile crisis numbers in each pastor office, and ongoing procedural training)
- domestic violence information + local shelter information on hand
- Train your prayer teams, welcome teams, childcare workers, homegroup leaders, etc.
Step 2: Create a “3-meeting guideline”
Many churches adopt a boundary like:
- you can meet 1–3 sessions for stabilization and spiritual care
- if symptoms are ongoing or complex, you refer for clinical treatment
(This helps prevent unintentional drift into long-term pseudo-therapy.) - be clear in the first meeting about scope, and also about mandated reporting
Step 3: Document internally (not clinical notes)
You don’t need therapy notes. But you do need:
- date, who met, basic topic, and whether referral was offered
- safety actions taken (if needed)
- follow-up plan
- I know this is meant for ministry leaders, but I think we all understand CYA. Document. Period.
Step 4: Collaborate—don’t compete
The best model is: church supports spiritually + clinician treats clinically.
This reduces burnout on ministry staff and increases safety for congregants.
Our Full Podcast related to this topic
Want Help Building This Into Your Church Culture?
At Steadfast Christian Counseling, we offer Trauma-Informed Church Trainings that teach:
- scope of practice
- how to triage and refer
- what to do with trauma disclosures
- how to build a local resource list and care pathway
📩 Training inquiries: connect@steadfastcc.com
🌿 Counseling in Charleston: www.steadfastchristiancounseling.com
📅 Free consultation: https://sccandcic.janeapp.com
💌 Steadfast Friday Email Club: https://link.mytherapyflow.com/widget/form/Zmgwx48V1NL9CkMdudLv